SF3B1 mutated (SF3B1mut) MDS is associated with increased ring sideroblasts (RS) and favorable outcome. IWG-PM proposed that SF3B1mut MDS be considered a distinct entity in the absence of other unfavorable features. However, not all SF3B1mut MDS have similar clinical course. Hotspot K700E SF3B1mut leads to aberrant splice junctions and large-scale mRNA downregulation by activating a cryptic splice site. The functional effects of SF3B1mut outside of K700E is not clear. The outcome can also be altered by concomitant gene mutations and karyotype. In this study, we studied the clinical-pathologic features and outcome in a single-institutional series of 94 SF3B1mut and 415 SF3B1wt MDS, and explored the differences between K700E and non-K700E subgroups.
All untreated MDS patients diagnosed over a 3-year duration who underwent NGS were selected. Overall survival was calculated from diagnosis to death/ last follow-up. Univariate (UVA) Cox proportional hazards regression was used to identify any association of variables with outcome followed by multivariate modeling (MVA) (p-value 0.200 cutoff).
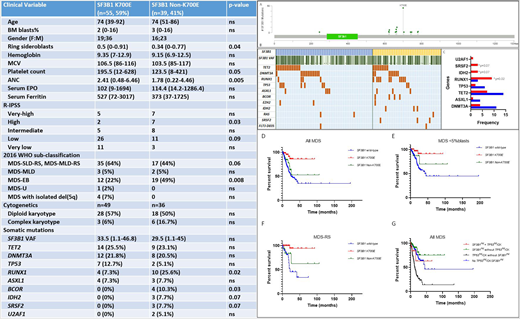
Of 509 patients, 94 (19%) had SF3B1mut: 59 men, 35 women; median age: 74 (39-92) years. Baseline characteristics: Table 1. Compared to SF3B1wt, SF3B1mut had a significantly higher median age (74 vs. 70, p=0.0008), MCV (105 vs. 96, p<0.0001), platelet count (188 vs. 78, p<0.0001) and lower BM blasts (2 vs. 4, p=0.003). SF3B1mut were less frequently therapy-related (18% vs. 34%, p=0.002), significantly enriched in R-IPSS VL/L and WHO MDS-RS and MDS with iso del(5q). Majority (~66%) had concomitant mutations: TET2 (25%), DNMT3A (21%), RUNX1 (15%), TP53 (10%), ASXL1 (7%), BCOR (4%), IDH1/2 (4%), SRSF2 (3%), RAS (3%) and EZH2 (3%) (Fig 1B). ~10% showed complex karyotype (CK). Among SF3B1mut, hotspot K700E mutation was seen in 55 (~60%). Non K700E mutations (n=39, 40%) frequently involved codons: H662, K666 and R625, seen in 8 patients each (Fig 1A). SF3B1 K700E showed a higher median RS% (50% vs. 34%; p=0.038), ANC (2.4 vs. 1.8, p=0.005) and a trend for higher platelet (196 vs. 124, p=0.05). SF3B1mut were less likely MDS-EB than non-K700E (22% vs. 49%, p=0.008). All 4 SF3B1mut patients that fit WHO criteria for MDS with isolated del(5q) had K700E (Table). The frequency of RUNX1 mutation was significantly higher in non-K700E cases (26% vs. 7.3%, p=0.012); mutations in BCOR (p=0.02), IDH2 (p=0.07) and SRSF2 (p=0.07) were exclusively noted in non-K700E cases (Fig 1C). There was no significant difference in TP53mut or CHIP-associated mutations DNMT3A, ASXL1 and TET2 or SF3B1 VAF. There was no significant differences in diploid vs. CK. However, K700E had lower CCCS categories (0/1, n=39; 2/3/4, n=10 vs. 0/1, n=19; 2/3/4, n=17); p=0.011).
Majority were treated with HMA [16/17 (94%) K700E; 15/19 (79%) non-K700, 217/ 277 (78%) SF3B1wt]. SF3B1mut had better OS than SF3B1wt in all MDS (NR vs. 25.2 months, p=0.0003; fig 1D), low-grade MDS (NR vs. 41.3 months, p=0.0015; fig 1E) and MDS-RS (NR vs. 22.3 months, p=0.0004; fig 1F). Four (7.3%) K700E died compared to 9 (23%; p=0.036) non-K700E. The outcome of non-K700E was similar to SF3B1wt, in all MDS, low-grade MDS and MDS-RS (median OS, NR for both; p=0.021). By UVA, the following associated with worse outcome: higher BM blasts, lower hemoglobin, platelet and MCV, prior chemo-radiation, CK, higher R-IPSS, absence of mutations in SF3B1 K700E, TET2 and U2AF1 and presence of TP53mut. Non-K700E did not associate with OS. By MVA, lower hemoglobin, higher R-IPSS, absence of SF3B1 K700E and presence of TP53mut were independent predictors of worse OS. Within MDS-RS categories, independent prognostic factors of worse OS included lower platelet, presence of mutations in non-K700E SF3B1mut, ASXL1, SRSF2 and TP53. TP53mut/CK was seen in 10% SF3B1mut MDS. No survival differences were noted between SF3B1mut with or without TP53mut/CK (median OS, NR) and SF3B1wt without TP53mut/CK (44.3 months), but TP53mut/CK with SF3B1wt MDS had a worse outcome (median OS, 12.9 months, HR 1.46, p=0.001; fig 1G). Same findings were noted within low-grade MDS and MDS-RS, suggesting SF3B1mut negates the poor prognostic effect of TP53mut/CK.
About 40% SF3B1mut MDS show non K700E mutations. K700E and non K700E SF3B1mut MDS show distinct clinical and mutational profiles, with K700E showing a significantly better OS compared to non K700E and SF3B1wt. Only SF3B1 K700E independently predicted for worse OS in MDS.
Sasaki:Pfizer Japan: Consultancy; Daiichi Sankyo: Consultancy; Novartis: Consultancy, Research Funding; Otsuka: Honoraria. Jabbour:Genentech: Other: Advisory role, Research Funding; BMS: Other: Advisory role, Research Funding; Pfizer: Other: Advisory role, Research Funding; AbbVie: Other: Advisory role, Research Funding; Takeda: Other: Advisory role, Research Funding; Adaptive Biotechnologies: Other: Advisory role, Research Funding; Amgen: Other: Advisory role, Research Funding. Kantarjian:Amgen: Honoraria, Research Funding; Ascentage: Research Funding; BMS: Research Funding; Daiichi-Sankyo: Honoraria, Research Funding; Immunogen: Research Funding; Jazz: Research Funding; Novartis: Honoraria, Research Funding; Pfizer: Honoraria, Research Funding; Sanofi: Research Funding; Actinium: Honoraria, Membership on an entity's Board of Directors or advisory committees; Adaptive biotechnologies: Honoraria; Aptitute Health: Honoraria; BioAscend: Honoraria; Delta Fly: Honoraria; Janssen: Honoraria; Oxford Biomedical: Honoraria; Abbvie: Honoraria, Research Funding. Garcia-Manero:Astex Pharmaceuticals: Consultancy, Honoraria, Research Funding; AbbVie: Honoraria, Research Funding; Bristol-Myers Squibb: Consultancy, Research Funding; Celgene: Consultancy, Honoraria, Research Funding; Merck: Research Funding; Onconova: Research Funding; Genentech: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Helsinn Therapeutics: Consultancy, Honoraria, Research Funding; Acceleron Pharmaceuticals: Consultancy, Honoraria; H3 Biomedicine: Research Funding; Amphivena Therapeutics: Research Funding; Novartis: Research Funding; Jazz Pharmaceuticals: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.